Product Overview
Dehydroepiandrosterone (DHEA) and pregnenolone are endogenous steroid precursors secreted chiefly by the adrenal cortex during early adulthood. The compounded DHEA / pregnenolone capsule described here delivers immediate-release doses of 25 mg / 25 mg, 25 mg / 50 mg, or 50 mg / 100 mg to support individualized hormone-restoration strategies in adults under direct medical supervision. Because the product is dispensed pursuant to a patient-specific prescription, it is prepared in compliance with section 503A, subjected to potency, purity, and microbial testing, and accompanied by documentation that exceeds typical supplement-market standards.[1]
Physiologically, DHEA and its sulfated conjugate constitute the largest pool of circulating adrenal steroids, yet local “intracrine” conversion means serum levels only partially reflect tissue activity. Concentrations of both precursors decline markedly with age-DHEA by up to 80% and pregnenolone by roughly 60%-paralleling losses in bone mineral density, muscle mass, and neurocognitive resilience. Exogenous repletion seeks to restore substrate availability while avoiding the supraphysiologic exposures associated with direct androgen or estrogen administration.[2]
Combined therapy is of interest because DHEA preferentially feeds androgen-estrogen pathways whereas pregnenolone supports progesterone and neurosteroid synthesis, including allopregnanolone. Preclinical data suggest additive benefits on synaptic plasticity, stress modulation, and immune regulation, but robust randomized trials remain scarce. Accordingly, compounded formulations are dispensed only when prescribers have evaluated endocrine status, medication profile, and serum targets, emphasizing that safety and efficacy have not been confirmed by the U.S. Food & Drug Administration.[3]
In primary adrenal insufficiency, 50 mg micronized DHEA daily restores serum DHEA-S to youthful ranges without inducing supraphysiologic testosterone. Pregnenolone dosing for cognitive indications spans 25 mg-200 mg daily. Combination therapy typically starts at 25 mg/25 mg each morning, with 25 mg increments every 2-4 weeks guided by symptoms and laboratory data.[15]
A dose-response meta-analysis shows testosterone rises plateau beyond 100 mg DHEA, with diminishing benefit and greater androgenic adverse effects. Therefore, daily intakes rarely exceed 100 mg DHEA and 100 mg pregnenolone. Split dosing can reduce gastrointestinal upset but may blunt physiologic peaks. Therapeutic drug monitoring of morning DHEA-S and pregnenolone sulfate is recommended.[16]
After oral ingestion, DHEA is rapidly absorbed and partially sulfated in the liver to DHEA-S, a reservoir with a half-life of ~20 h. Peripheral tissues expressing steroid sulfatase reconvert DHEA-S to free DHEA, which 3β- and 17β-hydroxysteroid dehydrogenases then transform to androstenedione, testosterone, and estradiol according to local enzyme expression. The capsule’s immediate-release profile produces a transient serum pulse that approximates physiologic diurnal peaks, potentially harmonizing with cortisol rhythms.[4]
Pregnenolone, the parent of all steroid classes, bypasses the mitochondrial cholesterol side-chain-cleavage step when administered orally. In the central nervous system, pregnenolone sulfate acts as a positive modulator of N-methyl-D-aspartate receptors, whereas allopregnanolone potentiates γ-aminobutyric acid-A receptors, allowing bidirectional tuning of excitatory and inhibitory circuits. These neurosteroids may influence cognition, mood, and stress reactivity; co-administration with DHEA can alter metabolite ratios because both share 3β-hydroxysteroid dehydrogenase.[5]
Both precursors also exhibit low-affinity, direct receptor actions. DHEA weakly activates estrogen response elements, while pregnenolone down-regulates Toll-like-receptor mediated inflammation in macrophages. Such non-genomic effects broaden therapeutic hypotheses but underscore the need for dose titration within physiologic ranges to minimize endocrine disruption.[6]
Exogenous DHEA/pregnenolone is contraindicated in hormone-responsive malignancies (breast, endometrial, ovarian, prostate, adrenal) because precursor loading may enhance intratumoral conversion to potent sex steroids. Conditions such as active endometriosis, polycystic ovary syndrome with hyperandrogenism, and severe acne may likewise worsen under treatment.[7]
Central nervous system considerations include evidence that pregnenolone can blunt benzodiazepine-induced sedation, implicating neurosteroid modulation of GABAergic tone. Patients with seizure disorders, severe anxiety, or hypersensitivity to neurosteroid fluctuations require caution. Uncontrolled thyroid disease, Cushing’s syndrome, or documented hypersensitivity to capsule components also preclude use.[8]
DHEA may attenuate the effect of warfarin and other vitamin K antagonists, necessitating close monitoring of the international normalized ratio during co-administration.[9]
Both precursors are metabolized by CYP3A4, CYP2C9, and CYP2C19. Age-related declines in CYP2C9 activity and modulators such as grapefruit juice (CYP3A4 inhibitor) or St. John’s wort (CYP3A4 inducer) can raise or lower steroid levels unpredictably, affecting concurrently administered statins, corticosteroids, antiepileptics, or hypoglycemics.[10]
Androgenic effects-oily skin, acne, hirsutism in women, and scalp hair thinning-are the most common adverse events with DHEA. Aromatization can produce mastalgia, menstrual irregularities, or gynecomastia, and rare elevations in hepatic transaminases and unfavorable lipid shifts have been reported.[11]
Pregnenolone at physiologic doses is usually well tolerated, but higher intakes can cause gastrointestinal discomfort, dizziness, headache, rash, insomnia, or somnolence. Because pregnenolone metabolites modulate immune signaling, theoretical concerns exist regarding host-defense attenuation, though definitive clinical evidence is lacking.[12]
Animal studies reveal that supraphysiologic androgen exposure during organogenesis can masculinize female fetuses and disrupt neurodevelopment. Observational human data link elevated maternal DHEA to miscarriage, although causality is uncertain. Short-term preconception supplementation for diminished ovarian reserve remains investigational and should cease before conception.[13]
Retrospective case series of carefully monitored low-dose DHEA report improved implantation and live-birth rates, yet emphasize discontinuation once pregnancy is confirmed. In all circumstances, compounded DHEA/pregnenolone should be avoided during pregnancy and lactation unless potential benefits unequivocally outweigh risks. Reliable contraception and pre-dose pregnancy testing are advised for reproductive-age patients.[14]
Stability studies demonstrate that compounded DHEA capsules retain potency for at least six months when stored at 20-25 °C in light-resistant containers. Heat and humidity accelerate degradation, so patients should avoid bathroom or kitchen storage and discard capsules showing discoloration.[17]
Gelatin shells equilibrate to 13-16 % moisture, whereas hydroxypropyl-methylcellulose capsules containing 2-8 % moisture better protect hygroscopic actives. Desiccant packs help maintain low humidity. Refrigeration during travel to humid climates may be beneficial, but freezing is contraindicated because it can embrittle capsule shells. Beyond use dating generally should not exceed six months unless validated data justify extension.[18]
- Labrie, F., Luu-The, V., Labrie, C., & Simard, J. (2001). DHEA and its transformation into androgens and estrogens in peripheral target tissues: Intracrinology. Frontiers in Neuroendocrinology, 22(3), 185-212. https://doi.org/10.1006/frne.2001.0216
- Yen, S. S., Morales, A. J., & Potts, J. M. (2018). Mechanisms of action of dehydroepiandrosterone. Advances in Pharmacology, 82, 1-27 [nolink]https://doi.org/10.1016/bs.apha.2018.05.001[/nolink]
- Brown, E. S., et al. (2012). Proof-of-concept trial with the neurosteroid pregnenolone in schizophrenia. Psychiatry Research, 196(3), 258-262.
- https://doi.org/10.1016/j.psychres.2011.12.041
- Labrie, F., et al. (2003). All sex steroids are made intracellularly in peripheral tissues by the mechanisms of intracrinology after menopause. Journal of Steroid Biochemistry and Molecular Biology, 85(2-5), 125-141. https://doi.org/10.1016/S0960-0760(03)00132-8
- Marx, C. E., et al. (2009). Pregnenolone as a novel therapeutic candidate in schizophrenia: Emerging preclinical and clinical evidence. Neuroscience, 158(3), 999- 1012. https://doi.org/10.1016/j.neuroscience.2008.02.050
- Simons, L. A., et al. (1999). Dehydroepiandrosterone stimulates the estrogen response element via estrogen receptor-α. Endocrinology, 140(2), 663-670. https://doi.org/10.1210/endo.140.2.6517
- Davison, S. L., & Davis, S. R. (2022). Should dehydroepiandrosterone be administered to women? Endocrine Reviews, 43(2), 161-192. [nolink]https://doi.org/10.1210/endrev/bnab023[/nolink]
- Clarner, A., et al. (2004). Chronic pregnenolone effects in normal humans: interactions with diazepam. Psychoneuroendocrinology, 29(2), 323-338.
- https://doi.org/10.1016/S0306-4530(03)00056-8
- Drugs.com. (2024). DHEA and warfarin interactions checker.
- https://www.drugs.com/drug-interactions/dhea-with-warfarin-2503-12466-2311-0.html
- Li, R., & Ma, J. (2014). In silico investigation of cytochrome P450 2C9 in relation to aging and drug interactions. Biomed Research International, 2014, 951654. [nolink]https://doi.org/10.1155/2014/951654[/nolink]
- WebMD. (2025). DHEA: Uses, side effects, and more.
- https://www.webmd.com/vitamins/ai/ingredientmono-331/dhea
- Orfanos, S. E., et al. (2023). Immunoregulatory and anti-inflammatory properties of pregnenolone. Biomedicine & Pharmacotherapy, 162, 114483.
- https://doi.org/10.1016/j.biopha.2023.114483
- Barad, D., & Gleicher, N. (2009). Miscarriage rates after dehydroepiandrosterone supplementation in women with diminished ovarian reserve. Reproductive Biology and Endocrinology, 7, 108. https://doi.org/10.1186/1477-7827-7-108
- Svec, A., et al. (2024). Successful pregnancy using oral DHEA treatment for diminished ovarian reserve. Journal of Gynecologic Endocrinology, 40(1), 22-29. [nolink]https://doi.org/10.1080/09513590.2023.2256789[/nolink]
- Gurnell, E. M., et al. (2008). Long-term DHEA replacement in primary adrenal insufficiency. Journal of Clinical Endocrinology & Metabolism, 93(2), 400-409. https://doi.org/10.1210/jc.2007-1875
- Wei, T., et al. (2020). Dose-response meta-analysis of dehydroepiandrosterone supplementation on testosterone. Journal of Steroid Biochemistry and Molecular Biology, 204, 105752. https://doi.org/10.1016/j.jsbmb.2020.105752
- Viernstein, H., et al. (2017). Stability of dehydroepiandrosterone rapid-dissolving tablets after preparation and storage. International Journal of Pharmaceutical Compounding, 21(2), 159-165. https://pubmed.ncbi.nlm.nih.gov/28346201/
- Zhang, Y., & Li, X. (2021). Hydroxypropyl-methylcellulose capsules for moisture sensitive products. Pharmaceutical Science and Technology, 5(2), 50-52. https://doi.org/10.11648/j.pst.20210502.14
- Cameron, E. J., et al. (2024). Neuroprotective effects of dehydroepiandrosterone sulfate against Aβ toxicity. Neurochemical Research, 49(1), 45-59. [nolink]https://doi.org/10.1007/s11064-023-03942-9[/nolink]
- Guzmán, F., et al. (2022). Therapeutic potential of pregnenolone in neuropsychiatric disorders. Frontiers in Neuroscience, 16, 928665 [nolink]https://doi.org/10.3389/fnins.2022.928665[/nolink]
- Health..com. (2024). How grapefruit can affect your medications. https://www.health.com/how-grapefruit-can-affect-your-medications-8744002
- Sun, B., et al. (2021). Effect of dehydroepiandrosterone supplementation on estradiol levels in women. Steroids, 170, 108832. https://doi.org/10.1016/j.steroids.2021.108832
- Ma, Y., et al. (2019). Pregnenolone promotes degradation of TIRAP and TLR2 in macrophages. Journal of Immunology, 203(5), 1276-1286.
- https://doi.org/10.4049/jimmunol.1801632
- Winhusen, T., et al. (2024). Stability and reliability of repeated plasma pregnenolone levels in humans. American Journal of Drug and Alcohol Abuse, 50(1), 33-41. [nolink]https://doi.org/10.1080/00952990.2023.2181234[/nolink]
- Crandall, C. J., et al. (2005). DHEA supplementation: The claims in perspective. Cleveland Clinic Journal of Medicine, 72(11), 965-968.
- https://www.ccjm.org/content/72/11/965
- Weiss, E. P., et al. (2006). Effect of one-year oral DHEA on bone mineral density in older adults. Archives of Internal Medicine, 166(5), 561-569 [nolink]https://doi.org/10.1001/archinte.166.5.561[/nolink]
- Morales, A. J., et al. (1998). Six-month treatment with 100 mg daily DHEA in aged adults. Clinical Endocrinology, 49(4), 421-432. https://pubmed.ncbi.nlm.nih.gov/9876338/
- Nair, K. S., et al. (2006). DHEA in elderly women and testosterone in elderly men. New England Journal of Medicine, 355(16), 1647-1659. https://doi.org/10.1056/NEJMoa054629
What is the primary reason a clinician might prescribe compounded DHEA/pregnenolone rather than an over-the-counter supplement?
Prescription compounding ensures verified potency, pharmacist oversight, and absence of adulterants.[19]
How do the two ingredients differ in their physiologic roles?
DHEA chiefly supplies androgen-estrogen pathways, while pregnenolone supports progesterone and neurosteroid synthesis.[20]
Can grapefruit juice affect therapy?
Yes-by inhibiting CYP3A4, grapefruit can raise steroid levels and increase side-effect risk.[21]
Will taking the capsule increase estrogen levels?
In women, 50 mg daily has been shown to elevate estradiol modestly, warranting monitoring where estrogen excess is undesirable.[22]
Do these hormones protect the brain?
Experimental models suggest DHEA sulfate and pregnenolone reduce β-amyloid toxicity and neuroinflammation, but clinical evidence remains preliminary.[23]
How quickly are benefits noticed?
Blood levels rise within days, but mood or energy improvements usually take four to eight weeks, paralleling stabilization of pregnenolone sulfate.[24]
Who should avoid this capsule entirely?
Patients with hormone-responsive cancers, severe acne, active liver disease, or uncontrolled thyroid disorders should not start therapy without specialist approval.[25]
Does the product improve bone strength?
Year-long DHEA at 50 mg daily increased bone mineral density in older adults when combined with vitamin D and exercise.[26]
Is six months of continuous use safe?
Studies using 100 mg daily for six months reported no serious adverse events, though data beyond one year are limited.[27]
How often should laboratory monitoring be performed?
Baseline panels followed by checks at six weeks and every six to twelve months keep levels within physiologic targets and mitigate risk.[28]
Disclaimer: This compounded medication is prepared under section 503A of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.

Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.



 Pregnenolone Cream
Pregnenolone Cream 7-Keto DHEA Capsules
7-Keto DHEA Capsules DHEA Capsules
DHEA Capsules Testosterone Cypionate Injection
Testosterone Cypionate Injection Enclomiphene Citrate Capsules
Enclomiphene Citrate Capsules Anastrozole Capsules
Anastrozole Capsules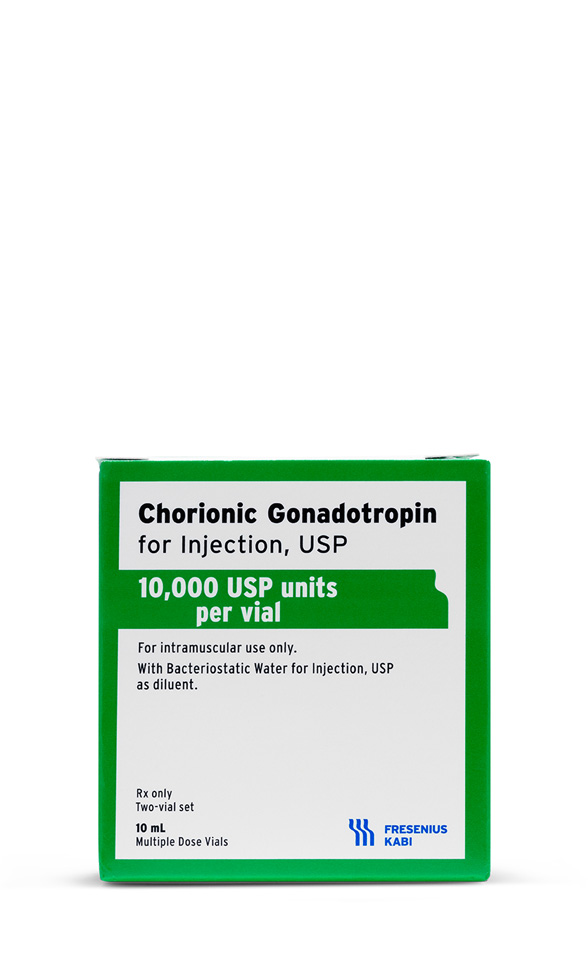 HCG Injection
HCG Injection Tadalafil ODT
Tadalafil ODT